I’m in the bathroom, door locked, staring at the mirror, stripped down to the heart-covered boxers my wife, Kathy, gave me for Valentine’s Day. As I hold the 0.5 cc syringe, I’m humming Neil Young’s “The Needle and the Damage Done” – a bit of black humour to pump up enough courage to jab the hypodermic into my abdomen.
My syringe is tipped with a hollow 31-gauge needle that’s not significantly bigger than a mosquito’s proboscis, so it’s not the stick, exactly, that I fear. (Well, maybe a little.) What scares me is the syringe’s contents: human chorionic gonadotropin, or hCG. It’s not an illegal steroid, nor is it growth hormone or testosterone, but it could still get me thrown out of pro sport. It is a natural glycopeptide hormone made in the placenta of a pregnant woman, extracted from her urine, and purified into the Pregny – made by pharmaceutical giant Merck – loaded into my syringe.
That’s correct: What I’m about to shoot up came from pee.
Why? You’re right to ask. As a drug, hCG is used as a fertility treatment. Since I’m blessed with three beautiful children already, I’m in no need of a sperm booster. Rather, the shot of hCG is to jumpstart my testes to produce more testosterone. The fact is, my T petrol tank is nearing E.
A simple blood test a month ago revealed that my total testosterone was lower than the 8 nmol/L considered low normal. A second test – considered more telling because it measures “free” testosterone, the type that binds with receptors all over the body and makes important stuff happen – returned an equally disturbing result.
My reading was “about the level of a boy just beginning puberty,” says endocrinologist Dr Florence Comite. Comite adds that for optimal functioning, free testosterone should be at least three times higher than my reading. Her statement hits me like a kick in the balls. Testosterone is what makes men men. It’s the fuel for muscle mass, bone density and body hair. It plays a supporting role in every major organ system, from your arteries to your brain.
Starting in his late 30s or early 40s, a man’s testosterone level begins to wane; research has shown that it drops by 1 to 2 percent a year after age 40. At that gradual rate, most men don’t notice the decline until they hit their 50s, when symptoms such as reduced energy, loss of libido and weaker erections start to appear, says Comite, the author of Keep It Up: The Power of Precision Medicine to Conquer Low T and Revitalize Your Life. The medical term is “hypogonadotropic hypogonadism,” but it’s also been described as “andropause” or even “male menopause”.
Me? Low Testosterone? Emasculated at age 52? It can’t be. I’m still relatively young and in better shape than many of my peers. While my libido may have dipped since my randier university days, it’s still strong. But I am doughier all around; I can’t bench-press 130kg anymore; long runs have become run/walks. Most importantly, I’ve learned that low testosterone is linked to diabetes and heart disease, both of which run in my family.
Options for Raising Testosterone
My pharmaceutical T-raising options are many: rub-on gels, testosterone injections, under-the-skin implants, hCG. I have no interest in topical treatments – testosterone can be transferred through skin contact, and I wouldn’t want to expose my wife or kids. Comite recommends hCG for guys like me whose bodies haven’t completely stopped making T, because hCG mimics luteinizing hormone, the natural “start” button for T production. She says it helps the body help itself by producing its own testosterone. This more natural approach with hCG is appealing. I wonder: If I can coax my cojones to make more testosterone, can that help me thrive into old age as well?
Comite is confident that it will, with many benefits that are increasingly supported by clinical science, such as . . .
Improved body composition. Reduced belly fat and more muscle are common outcomes of testosterone therapy. In a UCLA study conducted at seven US medical centres and published in the Journal of Clinical Endocrinology & Metabolism, men who were given T gel therapy added 2kg of muscle in six months, and 3kg over 18 months. “The improvement in body composition helps you metabolise sugar better and may help reverse insulin resistance,” says Comite.
Bone strength. When men are treated with testosterone, their bone mineral density increases, especially in their hips and spine. Osteoporosis is no longer considered a women’s disease; in fact, four out of 10 fractures due to brittle bones after age 50 occur in men.
Better sexual function. In a review of 17 studies in the journal Clinical Endocrinology, researchers found that an average of three months of testosterone supplementation boosted libido, increased the frequency of sex and triggered more nocturnal spontaneous erections.
A healthier cardiovascular system. Studies have found low testosterone levels in men with heart disease or with its risk factors, suggesting that T may play an important role in cardiovascular function. One theory: testosterone may help keep arteries flexible, allowing them to dilate and constrict with changes in blood flow.
We often write off saggy skin, a pot belly, heart disease and high blood sugar as normal aspects of ageing. If a needle prick of hCG can help me skip all that, I’ll take it willingly. And if I can feel stronger, sharper and more energetic into my 80s, hey, that’s a plus.
I wipe my skin with an alcohol swab, pinch my belly flab and plunge in the needle. It’s a mosquito bite, but I’m thinking this bug is my mate.
Age and Testosterone
As testing becomes more commonplace, the number of diagnoses of low T is rising. A study in JAMA Internal Medicine this year reported that between 2001 and 2011, the number of testosterone prescriptions written for men age 40 or older increased more than threefold. Younger men are asking for testosterone therapy as well, doctors report. “It has become gym jargon to ‘optimise testosterone,’ ” says urologist Dr Larry Lipshultz.
Pharmaceutical companies spent more than $100 million to promote treatments for low testosterone in 2012 alone. Some campaigns ask leading questions: “Could it be low T?”
This approach smacks of opportunism to doctors Lisa Schwartz and Steven Woloshin. In a JAMA Internal Medicine editorial earlier this year, they wrote, “Whether the campaign is motivated by a sincere desire to help men or simply by greed, we should recognise it for what it is: a mass, uncontrolled experiment that invites men to expose themselves to the harms of a treatment unlikely to fix problems that may be wholly unrelated to testosterone levels.”
Testosterone therapy is controversial because of the potential risks of long-term treatment – and the lack of any large, extended studies that convincingly establish its safety and efficacy. Wary doctors cite what they view as overblown claims of uncertain benefits, like increased energy, heightened sex drive and renewed vigour. They warn of under-appreciated risks, such as breast enlargement, testicle shrinkage, infertility, enlarged prostate, prostate cancer and heart attack. One 2010 randomised study of men using gel, reported in the New England Journal of Medicine, renewed debate. It was halted for safety reasons when some participants experienced cardiovascular problems, including heart attacks. However, advocates of testosterone therapy point to studies that found no connection to heart attack risk and that even suggested the treatment may promote heart health.
“Why buy any pig in a poke?” asks Dr Nortin Hadler, the author of Rethinking Aging. “You’re better off exercising than putting some silly compound in your armpit. Even though the product raises serum testosterone, who cares? It has no demonstrable, clinically meaningful benefit, so why expose your androgen-sensitive organs to any unnecessary risk?”
Even comedian Stephen Colbert has joined the T-therapy fray: “A man on TV is selling me a miracle cure that will keep me young forever. It’s called AndroGel . . . for treating something called low T, a pharmaceutical company–recognised condition affecting millions of men with low testosterone, previously known as getting older.”
Dr Abraham Morgentaler, an associate clinical professor of urology at Harvard Medical School, doesn’t believe that this “normal part of ageing” should be ignored. He regularly prescribes testosterone therapy at his practice. “Ageing is associated with bad hearing, bad teeth, bad arteries, bad joints and cancer, and we treat all those things,” he says. “Nobody would argue that you shouldn’t wear glasses because weaker eyesight is common as you get older.”
Cancer and Testosterone
Morgentaler’s line of reasoning makes me wonder: is injecting hCG any different from swallowing statin pills, as I do to help maintain my cholesterol profile? And what about the connection between testosterone elevation and prostate cancer that I’ve read about?
Consensus is hard to find. “There’s not one study showing that testosterone causes prostate cancer,” says Lipshultz. In a 2011 Journal of Urology study, both he and Morgentaler monitored men with untreated prostate cancer who were also on testosterone therapy for an average of two and a half years. After a year of monitoring, they found no signs of prostate cancer growth or worsening of symptoms.
Lipshultz and other doctors also worry about potential for abuse in the growing cottage industry of low-testosterone treatment centres that lure men with promises of anti-ageing and then don’t track their patients carefully enough. “The amount of testosterone in the circulatory system needs to be monitored to make sure it’s high enough to achieve benefits but not so high that it causes problems,” says Morgentaler.
As with many prescription-drug regimens, testosterone therapy has some downsides, including. . .
Reduced sperm production. The testes need to generate their own testosterone to make sperm; supplemental testosterone can suppress this natural production, which would be a concern for younger men who want to become fathers. (On a cosmetic note, it may also reduce testicular volume.)
Lower HDL (good) cholesterol. Or it may have no effect on it; results of studies on hypogonadal men so far have been mixed.
Higher red blood cell concentration. That’s good for athletic endurance, but it can thicken blood, which may produce clots – one more reason a man’s blood needs to be tested regularly during treatment.
I struggled with the choice to try hCG. I don’t like to mess with nature. And treatment is expensive. So I may be paying a high price for vague notions of libido energy and mood, and it may interfere with my ability to pay for other important stuff, like food and shelter. But avoiding disease would be worth the stretch.
I ultimately made my decision based on three factors. First and foremost, the lab results: my numbers backed up how I was feeling and my struggle against belly fat. Second, trust: Comite spent many years doing hormone research at the Yale School of Medicine and the National Institutes of Health. And she told me that 40 percent of her patients are doctors, who are pretty impressive as early adopters. Finally, the precision factor. Comite practises what’s called “precision medicine”: extensive diagnostics are used to evaluate patients and build personal programs to prevent diseases years before they manifest symptoms. While you might have 15 minutes of face time with your doctor during a typical visit, my physical checkup lasted three hours. Blood work was like happy hour for a vampire: I gave a dozen vials for testing. My lab reports totalled 11 pages and were filled with an alphabet soup of acronyms. Comite and her assistant pored over the results with me, explaining each finding (including pre-diabetes) and suggesting ways I could improve my numbers; an exercise physiologist gave me a customised workout and diet; I left with an armful of supplements.
The Latest Word
It has now been six months since I started hCG and the diabetes drug metformin. I swallow 10 supplement pills a day. I’ve completely cut out added sugar and severely rationed bread, biscuits and chips. I eat more broccoli. In the gym I’m pushing heavier weights and resting less.
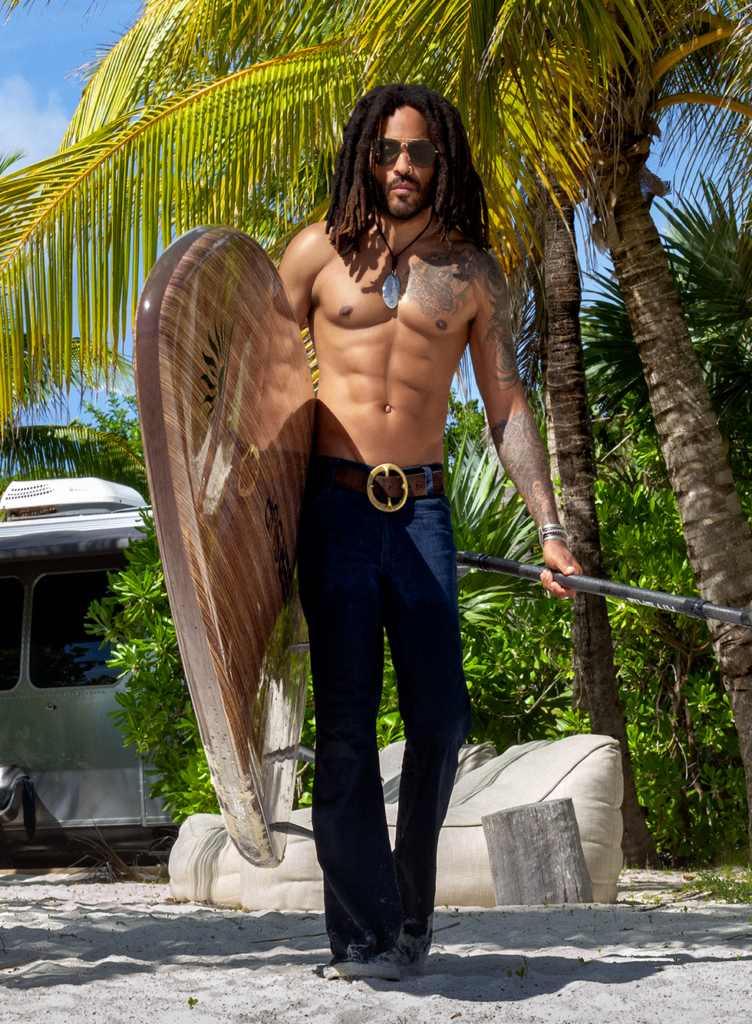
I’ve gained 2cm on my arms. I notice veins popping through tighter skin and my jeans are falling off me. People ask if I’ve lost weight. Actually, I’ve gained 2kg. A recent full-body scan showed why: in six months, I added 5kg of lean tissue (muscle) and lost 3kg of body fat, primarily in my belly. I know it hasn’t all been due to time in the weight room and clean living. I’m convinced the increase in testosterone has paid dividends.
I feel stronger and more energetic. My libido is about the same: healthy. Not 18-years-old healthy, but I’ve welcomed back morning wood. And my mood is better; I feel happier.
How I’m feeling could certainly be due to the placebo effect. But my test results aren’t fictional. They’re real. My total testosterone and free T have more than tripled – I’m no longer preadolescent.
At my six-month checkup, Comite said: “You’ve made some remarkable gains.”
How long will I stick with Comite’s testosterone-boosting plan? The benefits so far are overwhelmingly positive, and the more I research the risks, the less concerned I am.
Meanwhile, I’m enjoying the way I feel and the satisfaction of taking a proactive approach, one made possible by medical science. I think of my grandfather Janos, who couldn’t take advantage of the new technologies. His final years were spent sitting in a chair in pain, looking forward to his televised sports and a weekly shot of Wild Turkey. “Same as dead,” he’d say to me, resting his chin on his cane.
It’s a fate I’m unwilling to accept. If that means more testosterone for me, then hand over that syringe. Neil Young was wrong: The damage is done if I don’t shoot up.