You’ve seen the best athletes in the world do it, too. Photos of LeBron James with his knees wrapped in ice packs and his feet in a bucket of ice – and plenty of footage of top AFL and NFL players doing the same thing after matches. Tiger Woods used to talk about ice baths during his comeback to the PGA Championship. Heck, Kansas City Chiefs quarterback Patrick Mahomes recently appeared in a DirecTV commercial sitting in a tub of ice.
You think you’re doing it right, just like all those pros. But it’s been 50-plus years since Los Angeles Dodgers pitching legend Sandy Koufax appeared in a 1965 Sports Illustrated photograph with his left arm submerged in a vat of ice, an iconic moment in sport. Since then, no piece of published, peer-reviewed research has shown decisively that ice is beneficial to the healing process. In fact, many studies have shown the opposite. Ice can delay healing, increase swelling and possibly cause additional damage to injured tissues. That should stop you cold.
A BRIEF HISTORY OF WHERE WE WENT WRONG
The procedure for injury management followed by most doctors, physical therapists and athletic trainers hasn’t changed since 1978, when sports-medicine doctor Gabe Mirkin coined the phrase “the RICE protocol”. The acronym stands for rest, ice, compression and elevation. It’s taught in medical and physical-therapy schools and is listed on a host of medical websites as the top treatment for both acute and chronic sports injuries. Dr Rick Wright, a physician formerly with the St. Louis Blues, Cardinals and Rams, still swears by it.
“Ice is the best modality to control pain, swelling and inflammation, especially if you ice for 25-30 minutes so you get actual cooling of the tissue and decrease inflammation, as opposed to shorter periods where you can get a rebound response,” says Wright, who is currently the chair of the department of orthopaedic surgery at Vanderbilt University Medical Center. He believes nothing else has been definitively proven to work better.
Yet even Mirkin now disagrees. So much so that he co-wrote the foreword to the second edition of Gary Reinl’s 2013 self-published book, Iced! The Illusionary Treatment Option, which has become the bible of the growing anti-ice movement. “My RICE guidelines have been used for decades, but new research shows rest and ice actually delay healing and recovery,” says Mirkin, now 84.
Yes, if your muscles are sore, you can relieve that pain with ice. But the inflammation-causing that soreness is, in fact, bringing healing to the body; by icing, you “dampen that immune response,” he says. “You think you’re recovering faster, but science has shown you’re not.”
So how did Mirkin conceive RICE? Possibly, indirectly, thanks to a freckle-faced 12-year-old named Everett Knowles, who in 1962 tried to hop a freight train in Somerville, Massachusetts. As he did, his right shoulder smashed into a stone wall, severing his arm. The boy was rushed to Massachusetts General Hospital, where Harvard-educated surgeon Ronald Malt made a historic play: while deciding how to reattach Knowles’ arm – the first time such an operation would be successful – Malt put the appendage on ice.
Doctors began using the same protocol to treat all damaged tissue, especially in the sports world. Mirkin’s now-outdated book simply reported the anecdotal evidence. “In 1978, inflammation wasn’t even in researched literature, but everyone was resting, putting people in casts, wrapping things tightly with ice,” Mirkin says. There hadn’t been extensive research. And because RIC just wasn’t that catchy, and a gravitational assist can help the body reabsorb blood and fluid, Mirkin added an E at the end for elevation. It made for a fine slogan: “RICE is Nice”.

THE CASE AGAINST THE COLD
Remember when your school nurse told you to ice the ankle you rolled at recess? Did she tell you to chill it for five minutes? Ten? Twenty? Was it cubes in a bag or chips in a towel? Regardless, that nurse was right about exactly one thing: no study can dispute that ice is the cheapest, safest, and most readily available non-habit-forming way
to alleviate pain. But be warned. The pain will return once the tissue rewarms and the inflammatory response resumes.
That’s because this response needs to happen. The three stages of healing for soft-tissue injuries are now universally accepted by the medical community: inflammation, repair and remodelling. And you can’t reach the last two without phase one.
When tissue is damaged, the immune system initiates that inflammatory response. In 2010, a study published in The Federation of American Societies for Experimental Biology Journal showed that it’s necessary in order to heal damaged tissue and repair muscle in mice. The body deploys its repair and clean-up crew in the form of macrophages, a type of white blood cell that removes dead cell and tissue debris. They produce the protein called insulin-like growth factor 1, which is required for muscle repair and regeneration. So blocking the inflammatory response impedes healing by preventing the release of IGF-1. Ice does that by constricting blood vessels, allowing less fluid to reach the injured area. A 2013 study in The Journal of Strength and Conditioning Research found that topical cooling delays recovery from eccentric exercise-induced muscle damage. And a 2015 article in Knee Surgery, Sports Traumatology, Arthroscopy showed that the narrowing of blood vessels caused by icing persists after cooling ends. The resulting restriction can kill otherwise healthy tissue, adding more damage on top of the existing injury. Needless to say, that’s not a process that’s going to hasten your return to your favourite sport.
This isn’t just about serious injuries, either; it’s about the way you recover from workouts. Remember: having very sore quads because of a workout is different from having a torn quadriceps only by degrees.
A 2015 study published in The Journal of Physiology found that regular cold-water immersion after strength training – ice baths – substantially lessen long-term gains in muscle mass and strength by stunting the cell activity crucial for building stronger muscles. When you hit the cold tub after strength exercises, thinking you are reducing inflammation, what you’re doing instead is delaying recovery.
Inflammation and swelling have been deemed the enemy, but only swelling is actually bad. “When you recruit inflammatory markers to an acutely injured area, with that comes fluid,” says Dr Joshua Appel, an Air Force flight surgeon and the chief of emergency medicine at the Southern Arizona VA Health Care System. “The body knows how to heal itself, so you’re not getting too much fluid. But you can have not enough evacuation.”
COOL ALTERNATIVES TO ICE
How, then, does the body clear swelling? Most of the particles are too large to move through the vessels of the circulatory system, so they must instead be evacuated through the vessels of the lymphatic system. The lymphatics, though, are a passive system, fully reliant on muscle activation; movement is necessary to propel fluid through the vessels. Sitting still with an ice pack
creates the exact opposite effect. “With an acute injury, you want to get the good stuff in and the bad stuff out,” says Appel, who no longer uses ice to treat the countless
ankle and knee injuries suffered by his pararescue jumpers. “The only way to do that is through movement.”
Do you think our hunter-gatherer ancestors rolled their ankles, dug some ice out of a snowbank, sat down and stopped chasing dinner? It’s more likely that they forged on, and the movement facilitated healing.
Pushing a sprained ankle may sound ill-advised, but a 1999 study published in the Journal of the American Academy of Orthopaedic Surgeons showed that for those with musculoskeletal injuries or who have undergone surgery, loading damaged tissue – that is, applying force to it – actually accelerates healing for bone and muscle tissue.
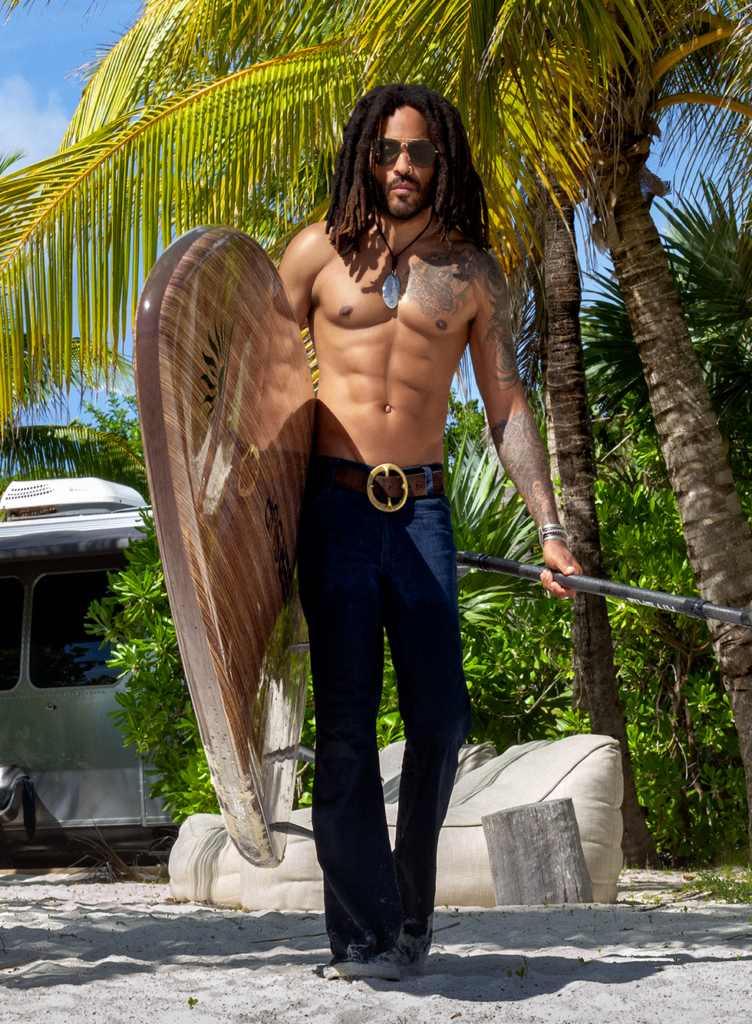
Moving sore muscles can be easy. Baseballer Corey Kluber, a two-time American League Cy Young Award winner, has iced his arm once in the past eight years. Instead, he does resistance exercises that target his rotator-cuff muscles after he pitches, naturally activating muscles and moving fluid out of damaged tissues. “When I was younger, I iced because that’s what people did; that’s what I was told to do,” Kluber says. “But over time, I realised I felt better not icing, because I always felt stiff when I did.” The result: Kluber says he can accomplish more the day after pitching.
Acute injuries are more complicated. No, you don’t want to squat 180 kilograms on a torn ACL. But let’s say you sprain your ankle. If your physical therapist clears you to stand on it, don’t hesitate to do so.
If an injury is too painful or the area is too fragile for any type of voluntary movement, consider using a neuromuscular electrical stimulation device (better known as NMES), says physical therapist and legendary mobility guru Kelly Starrett. Such devices (and there are plenty on the market) use small currents to create non-fatiguing muscle contractions, allowing waste and congestion to be removed by your lymphatic system.
Seven years ago, Starrett had a patient who’d had reconstructive ACL surgery and skipped ice for an NMES device. “We had no swelling 24 hours post-surgery,” he recalls. His patient’s range of motion and quadriceps control, which often take weeks to recover, were restored almost immediately. No swelling meant no pain. “We have to allow the body to excel at what it does automatically, which is heal,” Starrett says.
There are newer prescriptive acronyms. METH – movement, elevation, traction, heat – was coined in 2011 by Canadian exercise physiologist John Paul Catanzaro. In April last year, two Canadian physical therapists pushed PEACE (protect, elevate, avoid anti-inflammatory modalities, compress, educate) and LOVE (load, optimism, vascularisation, exercise) on the British Journal of Sports Medicine blog.
So, why do doctors and therapists still use ice? Sheer bad habit, speculates Chip Schaefer, the Chicago Bulls’ director of performance health, who won six NBA titles while icing everyone on Michael Jordan’s Bulls. He doesn’t anymore. “You’re always going to fall back to, ‘Well, I did this with Jordan, and he got better’,” he says. “But we try to pride ourselves on following evidence- based practice.”
Athletes are no different. Like you, many have been icing for as long as they can remember – and is a trainer really going to say no to LeBron’s request for ice?
But healing is the name of the game, and faster recoveries happen without ice. More and more people are realising that – and you should, too. Because the meltdown has already begun.
This article originally appeared in the May issue of Men’s Health, on sale now.
RELATED: The Most Effective Protein To Rebuild Muscle Lost During Injury